Abstract
Autoimmune hemolytic anemia (AIHA) and immune thrombocytopenia (ITP) are known autoimmune complications of chronic lymphocytic leukemia (CLL). Current literature has established that autoimmune cytopenias (AICs) secondary to CLL can arise prior to or in reaction to a therapy, such as Fludarabine, and therefore it is important to assess the roles novel therapies play with respect to autoimmune cytopenias.
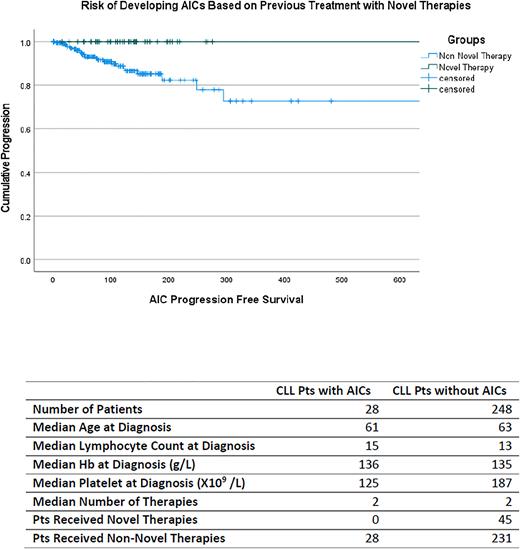
In this study we assessed the presenting characteristics and outcomes of patients (pts) with CLL who developed AICs. An electronic database search of 1056 patients with confirmed diagnosis of CLL who presented at St Paul's Hospital, Vancouver, Canada over 30 years and between 1991 and 2021 was performed with 520 having a complete data set. 276 pts (53%) who have undergone at least one treatment for their confirmed CLL presented with a full dataset. Of the 276 pts, 28 (10.1%) developed an autoimmune cytopenia secondary to CLL, with 20 pts developing AIHA, 5 pts developing ITP, and 3 pts developing both AIHA and ITP throughout the course of their treatments. Patients' characteristics are as detailed in the table. Time taken to develop an AIC (AIC Progression Free Survival) was then calculated using IBM SPSS and then incorporated into the Kaplan Meier method.
Patients who had taken a novel therapy (Ibrutinib, Acalabrutinib, Venetoclax) at any point prior to developing an AIC were defined as the novel-therapy group. Patients who had not received any novel therapy prior to developing an AIC were defined as the non novel therapy group. At 50 months, 11 pts in the non novel therapy group (4.9%) developed an AIC, while 0 of the pts (0%) in the novel therapy group developed an AIC. At 100 months, 16 pts in the non novel therapy group (7.1%) developed an AIC, while 0 of the pts in the novel therapy group developed an AIC (p=0.014). On bivariate analysis novel therapies maintained high significance as a preventative treatment, with the number of AIC diagnoses negatively correlating with the number of pts treated with novel therapies (p=0.011). Other possible predictive markers for AICs were evaluated through bivariate and multivariate analysis. On bivariate analysis, the development of AICs significantly correlated with an increase in the number of treatments the patient received due to increased disease progression (p=0.001). Multivariate analysis through cox regression shows that factors such as greater age at diagnosis, male gender, and the lack of treatment with novel therapies are significant predictors for development of AICs (P<0.05).
This study has demonstrated the significant preventative effect novel therapies can have on AICs in CLL. Incorporating novel therapies as a first line treatment presents as a reasonable strategy in reducing risk of AICs for patients that present with the other risk factors such as greater age at diagnosis and male gender.
Disclosures
Leitch:Abbvie: Honoraria, Membership on an entity's Board of Directors or advisory committees, Research Funding; Alexion: Honoraria, Membership on an entity's Board of Directors or advisory committees, Research Funding; BMS: Honoraria, Membership on an entity's Board of Directors or advisory committees, Research Funding; Celgene: Honoraria, Membership on an entity's Board of Directors or advisory committees, Research Funding; Fibrogen: Honoraria, Membership on an entity's Board of Directors or advisory committees, Research Funding; Forma: Honoraria, Membership on an entity's Board of Directors or advisory committees, Research Funding; Novartis: Honoraria, Membership on an entity's Board of Directors or advisory committees, Research Funding; Otsuka: Honoraria, Membership on an entity's Board of Directors or advisory committees, Research Funding; Taiho: Honoraria, Membership on an entity's Board of Directors or advisory committees, Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal